As the Cosmetic Medicine arena grows exponentially, practitioners are always (and should be) looking to expand their offering and exploring new ways to improve their practice.
At the same time, patients are becoming more discerning and are constantly looking for quality indicators and value-added benefits from their practitioner.
Whilst traditionally the focus has been on non-surgical skin treatments for ‘anti-ageing’, there has been a subtle paradigm shift to now discussing and treating ‘skin health’ in a more holistic fashion.
Mr Banwell’s personal ‘Skin Health Matrix’ includes not only the traditional modalities of advanced skin care (cosmeceuticals), microneedling, fillers and toxins, to name but a few, but also focuses on the important role of prevention and patient education in skin cancer.
Teaching patients about their skin, with a particular focus on sun safety and skin cancer can be, not only rewarding, but help reinforce the reasons for recommending ‘skin health’ treatments in the first place (with concomitant business benefits).
Furthermore, early recognition of pathological skin conditions is vital and cosmetic medicine (skin health) practitioners are in a unique position to screen, diagnose and refer.
When to treat or not to treat a pigmented patch on the face is a critical decision – for instance, recently Mr Banwell has had to manage someone who was having ‘cosmetic’ laser treatments on a melanoma for a couple of years!
Skin Cancer Facts
Skin cancer is the most common cancer in the Caucasian population (ahead of breast, lung and colon). In the UK there were over 85,000 non-melanoma skin cancers (NMSC) and over 11,000 melanoma skin cancers diagnosed in 2007.
If we compare these to the 2000 figures, where 62,200 NMSC were diagnosed, we can see an exponential increase. Furthermore, the WHO estimates over 130,000 newly diagnosed cases of melanoma worldwide per annum, a figure which is undoubtedly increasing due to continuing detrimental changes in the ozone layer and continuing lack of sun exposure precautions.
The American Association of Dermatologists have translated their estimations into plainer figures: in the US one person dies every hour from melanoma, a cancer that only represents 3% of all skin cancers in America. These figures are more worrying if we consider that melanoma can be treated if caught early.
If rates of skin cancer are rising, climatic impact intensifying and individual accountability remaining low, we have an expanding public health issue.
Currently Plastic Surgeons, Dermatologists and General Practitioners represent the main triad of education, identification and early treatment; however, perhaps it is cosmetic practitioners who should also be at the forefront of screening and patient education too as the majority of their patients are being treated for the effects of photodamage.
Skin Cancer Types
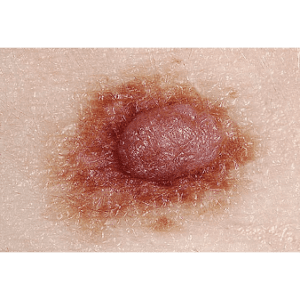
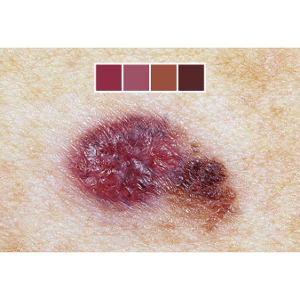
Skin cancer comprises both melanocytic and non-melanocytic lesions. NMSC includes Squamous Cell Carcinoma (SCC) and Basal Cell Carcinoma (BCC). SCC is often preceded by precursor lesions which have a metastatic risk of 0.5-3.3%.
Once a SCC is established, the metastatic risk ranges from 0.5-40%, whereas BCCs (the most common of all cancers) arise directly as slow growing, locally invasive lesions with an extremely low metastatic potential. Melanomas occur less frequently but carry higher risk of metastasis and death and may occur in the younger population (melanoma is the second most common cancer in the 20-39 age group).
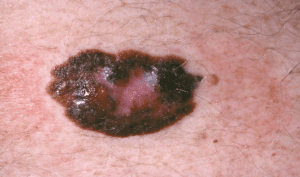
They often evolve from pigmented nevi (moles) but can initiate in any melanin (pigment)-containing tissue, particularly in areas of successive sun exposure. It is therefore the melanomas that need to be identified early as well as their precursor lesions – lentigo maligna and dysplastic naevi.
Table 1:
Seven point checklist for suspected malignant melanoma
Major signs
• If an existing mole gets larger or a new one is growing
• If the mole has an irregular outline
• If the colours are mixed shades of brown or black
Minor signs
• If the mole is bigger than the blunt end of a pencil
• If it is inflamed or has a reddish edge
• If it is bleeding, oozing or crusting
• If it starts to feel different: for example, itching or painful
What to look out for:
“What is most difficult of all? It is what appears most simple; to see with your eyes what lies in front of your eyes.” Goethe
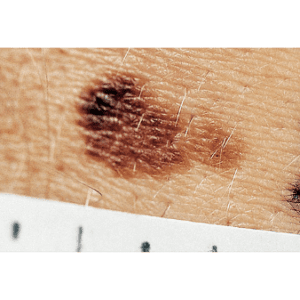
The Major and Minor signs mentioned in Table 1 can be a screening tool for suspected abnormal moles. However, an alternative schemata concentrates on pattern recognition – the so-called A,B,C, D,E approach -ASYMMETRY, BORDER, COLOUR, DIAMETER, ELEVATION.
Asymmetry means that one half of the mole does not match the other half
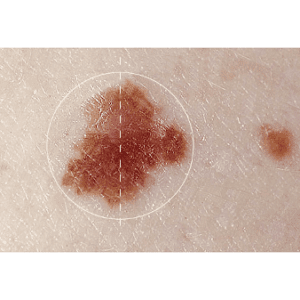
Borders may be ragged, altered or blurred
Different colours within the mole
Diameter – moles that are larger than a pencil should be checked out by a doctor and if necessary referred to a skin specialist. As a point of note, benign moles are usually less than 6mm in diameter
If moles change in size or become raised (Elevated) – refer!
Examples of skin cancer
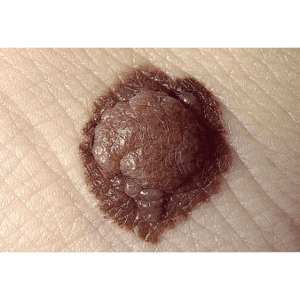
Melanoma
Squamous cell carcinoma
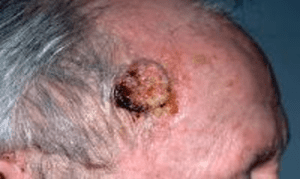
Basal Cell Carcinoma

Skin Cancer Aetiology
The development of photodamage and cutaneous malignancy is multifactorial and strongly related to UV exposure. Although all forms of UV radiation have carcinogenic potential, UVB is known to be more potent than UVA and effects damage directly on cellular DNA. Chronic sun exposure patterns are more associated with development of SCC, as opposed to episodic sun burning which is linked to development of dysplastic naevi and melanoma.
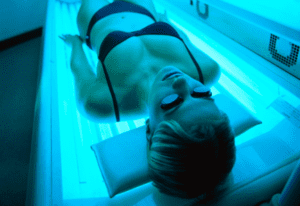
Other risk factors include increasing age, genetic susceptibility, immunosuppression, some cutaneous conditions and constitutional factors such skin colour (especially Fitzpatrick Skin types I & II) and number of typical and atypical nevi. Sun beds merit separate mention as they deliver intense, concentrated UV radiation and there is NO place for their use – a report by Cancer Research UK demonstrates an increased risk of melanoma of 75%!
Despite increased awareness of skin cancer and the need for modified behaviour to UV exposure, skin cancer rates continue to rise – it is therefore vital that we as health care professionals reinforce the important message of daily sun protection and use of SPFs.
SPFs are anti-ageing!

Have a higher index of suspicion in patients with lots of moles

Sun beds are a no-no
Premalignant Lesions
Premalignant lesions include Actinic Keratosis (AK) and Bowen’s disease (BD) which lie on a spectrum of photo-related lesions between photo-ageing and SCC. Of course, not all precursor lesions develop into invasive carcinoma.
AKs are the most common dysplastic epidermal lesions, with a prevalence of up to 60% of adults over 40 years old. They present as areas of crustiness which may exhibit cyclical episodes of falling off then re-occurring The risk of progression from a singular AK to malignancy is low; however, risk increases with the number of lesions and the degree of field change or regional photodamage.
AK can be graded on a clinical scale which can guide treatment such as cryotherapy, curettage or medical treatments. However, if these lesions recur despite these modalities it is likely they are more active and will require more urgent action with surgery. In comparison, Bowen’s disease is Squamous Cell Carcinoma In Situ (CIS) and will ultimately progress to invasive carcinoma if untreated. Bowen’s presents as red erythematous plaques with crusty areas and can sometimes be mistaken as psoriasis.
Actinic keratosis
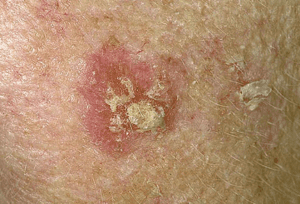

Bowens

Skin Cancer Treatment
The mainstay of treatment for skin cancers is usually definitive excisional skin cancer removal surgery but medical treatments (solarase, 5-fluorouracil, imiquimod and photodynamic therapy) are increasingly being employed for pre-malignant lesions (and for some skin cancer subtypes such as superficial BCCs).

Skin Cancer: Prevention
Despite effective treatments, prevention represents a key role of the cosmetic practitioner. Primary prevention through sun avoidance, use of protective products and education, is the most effective intervention in reducing the risk of photodamage.
Despite an established link between cutaneous malignancy and sun damage, there are still considerable failings in peoples’ attitudes. Sunscreen has been shown to reduce incidence of SCC and precursor lesions. Furthermore UVB-induced genetic point mutations have been identified in the development of BCC and SCC, suggesting reducing UVB skin radiation could reduce cancer development risk.
Studies emphasising the disparity between intentional sun protection use and actual application demonstrate the need for SPF to be included in daily moisturisers as part of national skin cancer prevention. Recent studies suggest we are still losing the behavioural battle as secondary school age students report poor sun protection use despite being well informed about skin cancer risk!
There is some good evidence to support use of topical products such as retinoids, antioxidants, vitamin C and E to reduce the carcinogenic potential of UV exposure. The evidence for use of cosmeceuticals and chemical peels to promote skin health and reduce the risk of malignant transformation is therefore gaining tremendous support.
Cosmetic Practitioners as gatekeepers
In response to the global increase in skin cancer, it is increasingly important for cosmetic practitioners to have an awareness of premalignant and malignant lesions, including metastatic risk. As treatment modalities broaden, the evidence for topical treatments in combination or as field therapy offers potentially more efficacious treatments, with excellent cosmetic effects. Additionally, accelerating trends combined with behavioural downfalls suggests we are all are not doing enough to emphasise the importance of the use of SPF and sun avoidance.
Ultimately, cosmetic practitioners are in an excellent position to promote skin cancer awareness and behavioural change secondary to patient education. Emphasising the importance of sun protection and the link between photoageing and skin cancer development is crucial – sun creams truly are anti-ageing!
Additionally, by keeping up to date with the beneficial effects of many cosmeceuticals and chemical therapies means practitioners can better inform treatment choices.
Lastly and perhaps most importantly, links with specialists in skin cancer (Plastic Surgeons or Dermatologists) will facilitate a streamlined pathway for your patients should any adverse pathology be picked up. This link and pathway inspires confidence in patients and can further enhance the quality and scope of your practice.







































25th June 2025
Bringing Confidence Forward: A Personal Look at Hairline Lowering Surgery
Read More
24th June 2025
Lip Lift Surgery: A Subtle Change That Speaks Volumes
Read More
3rd June 2025
Post-Surgery Compression Garments in Plastic Surgery
Read More